WHAT IS DEEP BRAIN
STIMULATION (DBS)?
David Ferrier and others in the 1880s showed
that direct electrical brain stimulation could change behavior and that
activation of specific regions correlated with certain behavioral changes. For
the past 100 years, neurosurgeons have stimulated the brain electrically during
brain surgery, cataloguing the resulting effects along the way. Physicians have
long known that electrical stimulation could be therapeutic as well. During
electroconvulsive therapy (ECT), a doctor applies electrodes directly to the scalp
of an anesthetized subject with the goal of inducing a generalized seizure. For
reasons that are still unclear, a repeated ECT session over the course of
several weeks is an effective treatment for depression, mania and catatonia.
Unfortunately, the technique is associated with memory loss and requires
repeated general anesthesia. Because the skull acts as a large resistor that
spreads direct electric current, ECT cannot be focused on or directed to
specific targets within the brain.
 Of late, neuroscientists have explored other methods to
electrically stimulate the brain. These new techniques tend to be either more
focused or less invasive, or both, than the older ones. Employed in conjunction
with the advanced brain-imaging technologies developed over the past two
decades, these approaches are being used to build on our recently assembled
understanding of how the brain works. Two direct electrical brain-stimulation
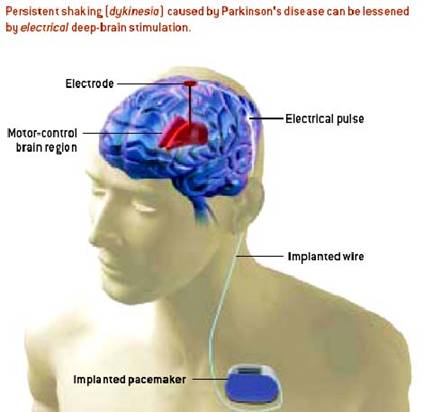
techniques have been approved for therapeutic use. In deep brain stimulation
(DBS), a neurosurgeon guides a small electrode into the brain through a small
hole in the skull with the help of three-dimensional images (left). The surgeon then
connects the electrode to a pacemaker (signal generator) implanted in the
chest. The pacemaker sends high- frequency electrical pulses directly into the
brain tissue.††††††††††††
Of late, neuroscientists have explored other methods to
electrically stimulate the brain. These new techniques tend to be either more
focused or less invasive, or both, than the older ones. Employed in conjunction
with the advanced brain-imaging technologies developed over the past two
decades, these approaches are being used to build on our recently assembled
understanding of how the brain works. Two direct electrical brain-stimulation
techniques have been approved for therapeutic use. In deep brain stimulation
(DBS), a neurosurgeon guides a small electrode into the brain through a small
hole in the skull with the help of three-dimensional images (left). The surgeon then
connects the electrode to a pacemaker (signal generator) implanted in the
chest. The pacemaker sends high- frequency electrical pulses directly into the
brain tissue.††††††††††††
DBS
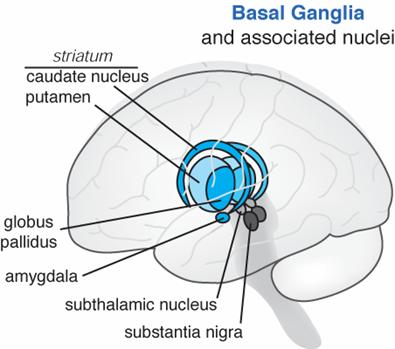
is approved by the U.S. Food and Drug Administration for the treatment of
Parkinsonís disease, typically in patients who no longer respond to
medication. Within the motor-control circuitry of the brain, several regions
(including the internal globus pallidus, thalamus and subthalamic nucleus) are
inhibitory in function and so act as brakes on movement.
 †
†
Schematic
of the Basal Ganglia of the Brain (left). X-Ray of patient with DBS lead in the
Subthalamic nuclei (right)
In current practice, neurosurgeons place DBS
electrodes in those regions and then stimulate them at high frequencies to
arrest the shaking (dyskinesia) that characterizes Parkinsonís. The technique
is being explored as a treatment
for depression as well. Little information exists concerning what happens
when DBS is applied to other brain regions or when low-frequency pulses are
used. †DBS electrodes can be removed with
no lasting damage. Thus, the procedure represents an advance over traditional
ablative brain surgery in which neural tissue is lost forever.